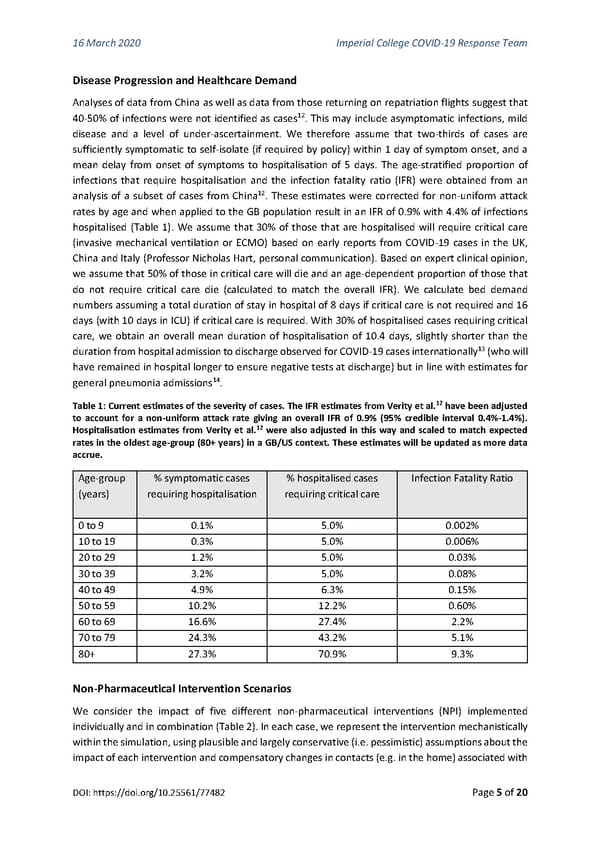
16 March 2020 Imperial College COVID-19 Response Team Disease Progression and Healthcare Demand Analyses of data from China as well as data from those returning on repatriation flights suggest that 12 40-50% of infections were not identified as cases . This may include asymptomatic infections, mild disease and a level of under-ascertainment. We therefore assume that two-thirds of cases are sufficiently symptomatic to self-isolate (if required by policy) within 1 day of symptom onset, and a mean delay from onset of symptoms to hospitalisation of 5 days. The age-stratified proportion of infections that require hospitalisation and the infection fatality ratio (IFR) were obtained from an analysis of a subset of cases from China12. These estimates were corrected for non-uniform attack rates by age and when applied to the GB population result in an IFR of 0.9% with 4.4% of infections hospitalised (Table 1). We assume that 30% of those that are hospitalised will require critical care (invasive mechanical ventilation or ECMO) based on early reports from COVID-19 cases in the UK, China and Italy (Professor Nicholas Hart, personal communication). Based on expert clinical opinion, we assume that 50% of those in critical care will die and an age-dependent proportion of those that do not require critical care die (calculated to match the overall IFR). We calculate bed demand numbers assuming a total duration of stay in hospital of 8 days if critical care is not required and 16 days (with 10 days in ICU) if critical care is required. With 30% of hospitalised cases requiring critical care, we obtain an overall mean duration of hospitalisation of 10.4 days, slightly shorter than the 13 duration from hospital admission to discharge observed for COVID-19 cases internationally (who will have remained in hospital longer to ensure negative tests at discharge) but in line with estimates for 14 general pneumonia admissions . Table 1: Current estimates of the severity of cases. The IFR estimates from Verity et al.12 have been adjusted to account for a non-uniform attack rate giving an overall IFR of 0.9% (95% credible interval 0.4%-1.4%). Hospitalisation estimates from Verity et al.12 were also adjusted in this way and scaled to match expected rates in the oldest age-group (80+ years) in a GB/US context. These estimates will be updated as more data accrue. Age-group % symptomatic cases % hospitalised cases Infection Fatality Ratio (years) requiring hospitalisation requiring critical care 0 to 9 0.1% 5.0% 0.002% 10 to 19 0.3% 5.0% 0.006% 20 to 29 1.2% 5.0% 0.03% 30 to 39 3.2% 5.0% 0.08% 40 to 49 4.9% 6.3% 0.15% 50 to 59 10.2% 12.2% 0.60% 60 to 69 16.6% 27.4% 2.2% 70 to 79 24.3% 43.2% 5.1% 80+ 27.3% 70.9% 9.3% Non-Pharmaceutical Intervention Scenarios We consider the impact of five different non-pharmaceutical interventions (NPI) implemented individually and in combination (Table 2). In each case, we represent the intervention mechanistically within the simulation, using plausible and largely conservative (i.e. pessimistic) assumptions about the impact of each intervention and compensatory changes in contacts (e.g. in the home) associated with DOI: https://doi.org/10.25561/77482 Page 5 of 20
 Non-Pharmaceutical Interventions to reduce COVID-19 mortality and healthcare demand Page 4 Page 6
Non-Pharmaceutical Interventions to reduce COVID-19 mortality and healthcare demand Page 4 Page 6